
Special tests for low back pain are essential diagnostic tools to identify underlying causes, guiding accurate diagnosis and effective treatment plans for patients.
Overview of Low Back Pain and Its Prevalence
Low back pain is a prevalent condition affecting millions worldwide, often stemming from musculoskeletal issues. It can result from injuries, poor posture, or chronic conditions like arthritis. The prevalence is high, making it a leading cause of healthcare visits. Understanding its causes and impact on daily life is crucial for effective management and reducing its societal burden.
Importance of Special Tests in Diagnosing Low Back Pain
Special tests play a crucial role in diagnosing low back pain by identifying specific pathologies and guiding targeted treatments. These tests help differentiate between various causes, such as disc herniation or nerve compression. They enhance clinical evaluation, ensuring accurate diagnoses and preventing unnecessary interventions. Regular use of these tests in clinical practice improves patient outcomes by addressing root causes effectively.
Categories of Special Tests for Low Back Pain
Special tests are categorized into physical examination techniques, diagnostic imaging, and provocation or functional tests to accurately diagnose the source of pain.
Physical Examination Techniques
Physical examination techniques involve assessing posture, range of motion, and palpation for tenderness or muscle spasms. These methods help identify structural abnormalities or soft tissue issues contributing to low back pain. Posture assessment reveals misalignments, while range of motion testing evaluates flexibility and mobility. Palpation allows clinicians to detect areas of tenderness, muscle spasms, or bony abnormalities, providing insights into the underlying cause of pain. These techniques are foundational in guiding further diagnostic steps.
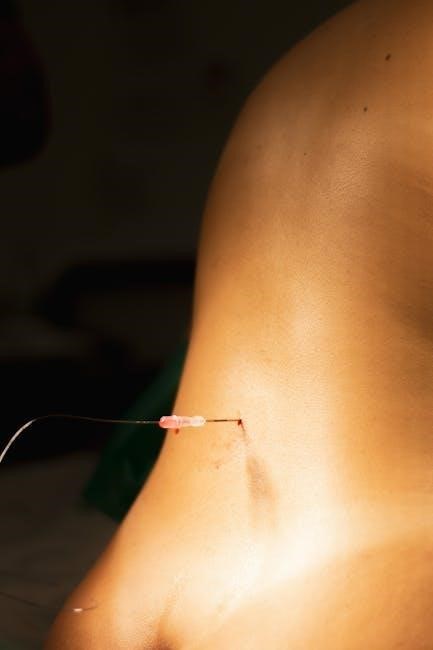
Diagnostic Imaging and Electrophysiological Tests
Diagnostic imaging, such as X-rays, MRI, and CT scans, provides detailed visuals of spinal structures to identify issues like herniated discs or fractures. Electrophysiological tests, including EMG and nerve conduction studies, assess nerve function and detect conditions like nerve compression. These tests are crucial for confirming diagnoses when physical exams and patient history are inconclusive, ensuring appropriate treatment plans are developed based on precise findings.
Provocation and Functional Tests
Provocation tests, such as the straight leg raise, assess pain reproduction by mimicking symptoms through specific movements. Functional tests evaluate range of motion, strength, and flexibility to identify limitations. These tests help differentiate between various pathologies, guiding targeted interventions. They are essential for confirming diagnoses and monitoring progress, ensuring personalized treatment plans address both pain and functional impairments effectively.
Key Special Tests for Low Back Pain
The straight leg raise, femoral nerve stretch, extension, and FABER tests are crucial for diagnosing lumbar pathologies, focusing on nerve root irritation and sacroiliac dysfunction.
Straight Leg Raise Test (SLR)
The Straight Leg Raise Test is a widely used assessment for diagnosing nerve root compression, particularly sciatica. During the test, the patient lies supine while the examiner lifts one leg to 60-90 degrees without bending the knee. Pain radiating below the knee, especially between 30-70 degrees, indicates a positive result, suggesting nerve root irritation, commonly associated with herniated discs. This test is highly specific and sensitive for identifying lumbar disc pathologies, making it a cornerstone in clinical evaluations.
Crossed Straight Leg Raise Test
The Crossed Straight Leg Raise Test is an advanced diagnostic tool used to assess nerve root compression, particularly in cases where the patient’s symptoms are unilateral. During the test, the asymptomatic leg is raised to identify if pain is provoked in the symptomatic leg. A positive result indicates nerve root irritation, often associated with disc herniation, commonly at the L4-L5 or L5-S1 levels. This test is highly specific and aids in confirming the presence of nerve root compression, guiding further diagnostic and therapeutic interventions effectively.
Femoral Nerve Stretch Test
The Femoral Nerve Stretch Test is used to assess femoral nerve irritation or compression, often related to lumbar disc herniation or spondylolisthesis. The patient lies prone, and the examiner passively extends the hip while flexing the knee. A positive test is indicated by tightness or pain in the anterior thigh or groin. This test is highly specific for identifying nerve root compression at the L2-L4 levels, aiding in the differential diagnosis of low back pain and guiding appropriate treatment strategies.
Extension Test
The Extension Test assesses for lumbar spine instability or discomfort during backward bending. The patient stands and extends their lumbar spine while the examiner applies gentle pressure. Pain or stiffness in the lower back during this movement may indicate conditions like spondylolisthesis or spinal stenosis. This test is valuable for identifying mechanical causes of low back pain and guiding further diagnostic or therapeutic interventions tailored to the patient’s specific condition.
FABER Test (Patrick’s Test)
The FABER Test (Patrick’s Test) is used to assess hip joint pathology or sacroiliac dysfunction. The patient lies supine with the leg placed in a figure-four position. The examiner applies downward pressure to the knee while stabilizing the opposite ilium. Pain in the groin or sacroiliac area indicates a positive result, suggesting potential hip arthritis, labral tear, or sacroiliac dysfunction. This test helps differentiate hip-related pain from lumbar spine issues, aiding in targeted treatment planning for the patient’s specific condition.
Role of Physical Examination in Low Back Pain
Physical examination is crucial for assessing posture, movement, and tenderness in low back pain. It helps identify musculoskeletal issues and guides targeted treatment strategies effectively.
Posture Assessment and Range of Motion
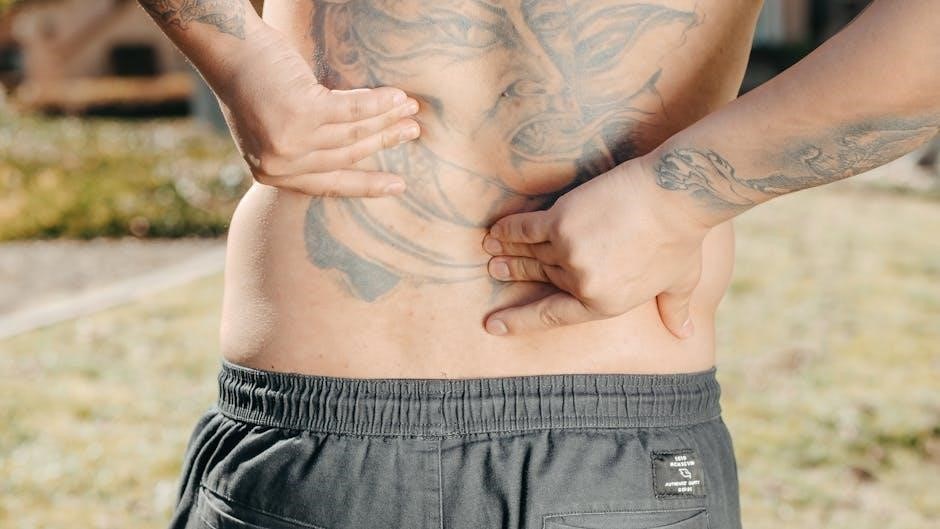
Posture assessment evaluates spinal alignment and structural abnormalities. Range of motion tests measure flexibility and movement in the lumbar spine. These evaluations help identify restrictions or imbalances that may contribute to low back pain. By observing how a patient stands, sits, and moves, healthcare providers can detect deviations from normal posture, such as lordosis or kyphosis. Limited or painful movement during range of motion tests can indicate underlying issues like muscle strain or joint dysfunction, guiding further diagnostic steps and treatment plans effectively;
Palpation for Tenderness and Muscle Spasm
Palpation involves gentle pressure to identify areas of tenderness and muscle spasms in the lumbar region. This technique helps pinpoint pain sources and detect soft tissue abnormalities. By examining the lumbar spine, healthcare providers can assess muscle tone and joint alignment, aiding in the diagnosis of conditions like muscle strain or nerve irritation. Palpation is a vital component of the physical exam, providing insights into the underlying causes of low back pain and guiding further diagnostic steps.
Reflex Testing and Neurological Evaluation
Reflex testing assesses nerve function by evaluating responses such as knee jerk and Achilles tendon reflexes. These tests help identify nerve root compression or neurological deficits. A neurological evaluation includes strength testing, sensory assessment, and gait analysis to detect motor or sensory impairments. Abnormal reflexes or neurological signs may indicate conditions like sciatica or nerve damage. This evaluation is crucial for pinpointing the origin of low back pain and guiding appropriate treatment strategies.

Diagnostic Tests for Low Back Pain
Diagnostic tests include imaging studies like X-rays, MRI, and CT scans, and electrophysiological tests such as EMG and nerve conduction studies to identify the pain’s underlying cause.
Imaging Studies (X-rays, MRI, CT Scan)
Imaging studies are crucial for diagnosing structural abnormalities causing low back pain. X-rays detect bony issues like fractures or degeneration. MRI provides detailed images of soft tissues, including discs and nerves, while CT scans offer cross-sectional views of the spine. These tests help identify herniated discs, spinal stenosis, or spondylolisthesis, guiding targeted treatment plans.
Electrophysiological Tests (EMG, Nerve Conduction Studies)
Electrophysiological tests like EMG and nerve conduction studies assess nerve function in low back pain cases. EMG measures muscle electrical activity to detect nerve damage or dysfunction. Nerve conduction studies evaluate signal speed and strength, identifying nerve compression or neuropathy. These tests are vital for diagnosing conditions such as sciatica or radiculopathy, ensuring precise treatment plans are developed based on nerve involvement.

Clinical Guidelines for Low Back Pain Management
Clinical guidelines emphasize evidence-based practices for managing low back pain, focusing on personalized treatment plans and formulation of specific diagnostic questions to ensure accurate care.
Best Practices for Chronic Pain Management
Best practices for managing chronic low back pain emphasize a multidisciplinary approach, including non-pharmacological interventions like physical therapy and psychological support. Guidelines recommend personalized treatment plans, focusing on improving function and reducing pain intensity. Patient education and self-management strategies are crucial, alongside regular follow-ups to monitor progress and adjust therapies. These practices align with evidence-based recommendations to enhance quality of life for individuals with chronic pain, ensuring comprehensive and effective care.
Evidence-Based Practice and Formulating Diagnostic Questions
Evidence-based practice involves using the best available research to guide clinical decisions, ensuring effective and efficient care for low back pain. Formulating focused diagnostic questions helps clinicians identify the most relevant tests and interventions. This approach aligns with clinical practice guidelines, promoting accurate diagnosis and treatment. By integrating patient history, physical exams, and special tests, healthcare providers can develop targeted plans, improving patient outcomes and reducing unnecessary procedures. Clear, evidence-based questions are key to optimal low back pain management.
Accurate diagnosis and targeted interventions are crucial for managing low back pain, ensuring improved patient outcomes and enhanced quality of life through evidence-based practices.
Importance of Accurate Diagnosis and Treatment
Accurate diagnosis and treatment of low back pain are crucial to prevent chronic pain, improve quality of life, and reduce healthcare costs. Early identification of underlying causes ensures targeted interventions, minimizing unnecessary treatments. Special tests guide clinicians in formulating effective plans, addressing both physical and emotional aspects of pain. Timely and precise care can prevent complications, enhance recovery, and restore functional abilities, emphasizing the need for a comprehensive and evidence-based approach in managing low back pain effectively.